Pancreatic Cancer
Everything You Need To Know About Pancreatic Cancer
Pancreas in the digestive system
The pancreas in the digestive system opens the pop-up dialog pancreatic cancer
Pancreatic cancer opens a pop-up dialog
Pancreatic cancer starts in the pancreatic tissue-an organ in the lower part of the abdomen. The pancreas releases enzymes that help digestion and produces hormones that help control blood sugar.
There are several types of growths in the pancreas, including cancerous and non-cancerous tumors. The most common type of cancer in the pancreas begins with cells that line the ducts that carry digestive enzymes out of the pancreas (pancreatic ductal adenocarcinoma).
In the early stages of cure, pancreatic cancer is rarely detected. This is because it usually causes symptoms after it has spread to other organs.
Choose a treatment plan for pancreatic cancer based on the degree of cancer. Options can include surgery, chemotherapy, radiation therapy or a combination of these.
Symptoms
The signs and symptoms of pancreatic cancer usually do not appear until the disease has progressed. They may include:
- Abdominal pain spreading to your back
- Loss of appetite or unexpected weight loss
- Yellow skin, white eyes (jaundice)
- Light stool
- Dark urine
- Itchy skin
- New diagnoses of diabetes or existing diabetes are becoming increasingly difficult to control
- Blood clot
- Fatigue
When to see the doctor
Pancreatic cancer treatment
If you experience any unexplainable symptoms that worry you, please see your doctor. Many other conditions can also cause these symptoms, so your doctor may check for these conditions as well as pancreatic cancer.
Reason
If you’re asking about why pancreatic cancer develops, it is due to genetic mutations that cause uncontrolled cell growth in the pancreas. These mutations can be inherited or acquired due to risk factors like smoking, chronic pancreatitis, obesity, and diabetes.
If you’re asking about why pancreatic cancer is difficult to detect and treat, it’s because:
- Lack of Early Symptoms – The pancreas is deep inside the body, so tumors often go unnoticed until they grow large or spread.
- Aggressive Nature – It spreads quickly to nearby organs like the liver and lungs.
- Limited Treatment Options – Many cases are diagnosed at later stages when surgery is no longer an option.
- Resistance to Therapy – Pancreatic cancer cells often do not respond well to chemotherapy or radiation.
Make An Appointment
Other type of Cancer
Know your pancreas
Your pancreas is about 6 inches (15 cm) long and looks like a pear lying on its side. It releases (secretes) hormones, including insulin, to help your body process sugar in the food you eat. It produces digestive juice to help your body digest food and absorb nutrients.
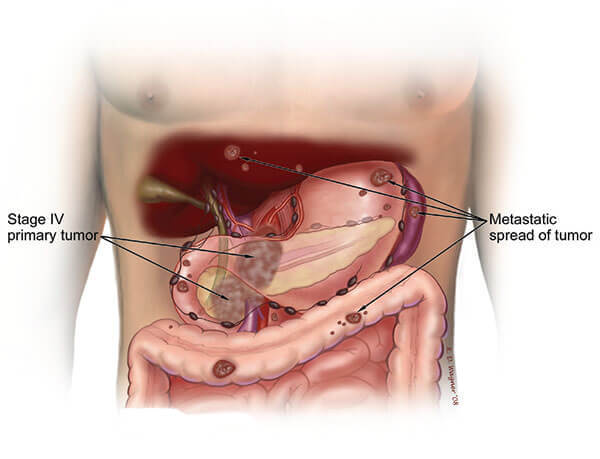
How pancreatic cancer develops
Pancreatic cancer occurs when the DNA of cells in the pancreas changes (mutations). The DNA of a cell contains instructions that tell the cell what to do. These mutations tell cells to grow out of control and continue to survive after normal cells die. These accumulated cells can form tumors. If left untreated, pancreatic cancer cells can spread to nearby organs and blood vessels as well as distant parts of the body.
Most pancreatic cancers start in cells in the pancreatic duct. This type of cancer is called pancreatic adenocarcinoma or exocrine pancreatic cancer. In the hormone-producing cells or neuroendocrine cells of the pancreas, the possibility of cancer formation is reduced. These types of cancer are called pancreatic neuroendocrine tumors, pancreatic islet cell tumors, or pancreatic endocrine cancers.
Risk Factors
Factors that may increase the risk of pancreatic cancer include:
- Smokes
- diabetes
- Chronic inflammation of the pancreas (pancreatitis)
- Family history of genetic syndromes that may increase the risk of cancer, including BRCA2 gene mutations, Lynch syndrome, and familial atypical mole melanoma (FAMMM) syndrome
- Family history of pancreatic cancer
- obesity
- Older age, because most people are diagnosed after 65
- A large study showed that smoking, long-term diabetes and poor diet increase the risk of pancreatic cancer, not just the risk of any of these factors.
- complication
- ERCP program
Endoscopic retrograde cholangiopancreatography opens a pop-up dialog
As pancreatic cancer progresses, it may cause complications such as:
lose weight. Many factors can cause weight loss in patients with pancreatic cancer. Weight loss may occur as cancer consumes energy in the body. Nausea and vomiting caused by cancer treatment or pressure on the stomach can make it difficult to eat. Otherwise, your body may have difficulty processing the nutrients in food because your pancreas cannot produce enough digestive juices.
jaundice. Pancreatic cancer that blocks the liver and bile ducts can cause jaundice. Signs include yellowing of the skin and eyes, dark urine and light colored stools. Jaundice usually occurs without abdominal pain.
Your doctor may recommend placing a plastic or metal tube (stent) in the bile duct to keep it open. This is done with a procedure called endoscopic retrograde cholangiopancreatography (ERCP). During ERCP, the endoscope will pass from your throat through the stomach and into the upper small intestine. The dye is then injected into the pancreatic duct and bile duct through a small hollow tube (catheter) that passes through the endoscope. Finally, take an image of the pipeline.
Pain
The growing tumor may compress the nerves in your abdomen, causing pain to worsen. Pain medicine can make you feel more comfortable. Therapies such as radiation therapy and chemotherapy may help slow tumor growth and reduce pain.
In severe cases, your doctor may recommend injecting alcohol into the nerves that control abdominal pain (plexus block). This process prevents nerves from sending pain signals to your brain.
Intestinal Obstruction
Pancreatic cancer that grows or is compressed in the first part of the small intestine (duodenum) prevents digested food from flowing from the stomach to the intestine.
Your doctor may recommend placing a test tube (stent) in your small intestine to keep it open. In some cases, surgery to place a temporary feeding tube or attach your stomach to the lower part of the intestine that is not blocked by cancer may help.
Prevention
Frequently Asked Questions
The pancreas is an organ in your abdomen that is located behind the bottom portion of your stomach. Pancreatic cancer starts in the tissues of the pancreas. Your pancreas generates hormones that help you control your blood sugar as well as enzymes that help with digestion.
The pancreas can develop both malignant and non-cancerous tumours, among other growths. The cells that lining the ducts that expel digestive enzymes from the pancreas are where the most prevalent kind of pancreatic cancer first develops (pancreatic ductal adenocarcinoma).
Rarely is pancreatic cancer found in its earliest stages, when it is most treatable. This is due to the fact that symptoms frequently don’t appear until the disease has progressed to other organs.
The stage and location of your pancreatic cancer, as well as your general health and personal preferences, will all affect how you are treated. When feasible, the primary objective of pancreatic cancer treatment for most patients is to eradicate the disease. The emphasis may shift to enhancing your quality of life and preventing the cancer from spreading or harming you if that isn’t a possibility.
Surgery, radiation, chemotherapy, or a combination of these may be used as treatments. Palliative care is the emphasis of therapy when pancreatic cancer has advanced and these therapies are unlikely to be beneficial. The goal of palliative care is to make you as comfortable as possible for as long as possible.
The exact etiology of pancreatic cancer is unknown. The risk of this form of cancer may be influenced by a number of variables, including smoking and some hereditary gene alterations.
You may be more susceptible to developing pancreatic cancer if you have:
- Smoking
- Diabetes
- Chronic inflammation of the pancreas (pancreatitis)
- Family history of certain genetic abnormalities, such as Lynch syndrome, familial atypical mole-malignant melanoma (FAMMM) syndrome, and the BRCA2 gene mutation, which can raise the chance of developing cancer
- Family history of pancreatic cancer
- Obesity
- Older age, as most people are diagnosed after age 65
An extensive study found that having diabetes for a long time, smoking, and eating poorly together increase the risk of pancreatic cancer more than any one of these factors would.
Your doctor could have you go through one or more of the following tests if they have a suspicion that you have pancreatic cancer:
- Imaging tests that create pictures of your internal organs. These exams aid in the visualization of your internal organs, including the pancreas, by your specialists. Ultrasound, computed tomography (CT) scans, magnetic resonance imaging (MRI), and, occasionally, positron emission tomography (PET) scans are methods used to diagnose pancreatic cancer.
- Using a scope to create ultrasound pictures of your pancreas. An ultrasound machine is used during an endoscopic ultrasonography (EUS) to create pictures of your pancreas from within your belly. The pictures are obtained by passing the gadget down your throat and into your stomach using a small, flexible tube called an endoscope.
- Removing a tissue sample for testing (biopsy). A biopsy is a process to take a little sample of tissue for microscopic analysis. During EUS, the tissue is often harvested by inserting specialized equipment via the endoscope. Less frequently, a needle is inserted through your skin and into your pancreas to retrieve a sample of tissue (fine-needle aspiration).
- Blood test. Your doctor may do a blood test to check for certain proteins (tumour markers) that pancreatic cancer cells secrete. CA19-9 is the name of one tumor marker test used to diagnose pancreatic cancer. Understanding how the cancer reacts to therapy may be useful. The test is less useful since some individuals with pancreatic cancer do not have increased CA19-9 levels, therefore it is not always accurate.
