Gynecologic Cancer
Everything You Need To Know About Gynecologic Cancer
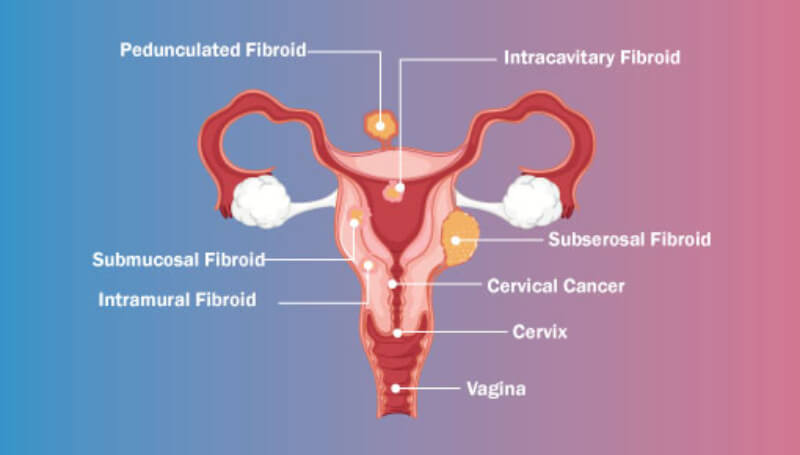
Types of Gynecologic Cancer
- Cervical cancer begins in the cervix, which is the lower, narrow end of the uterus. (The uterus is also called the womb.)
- Ovarian cancer begins in the ovaries, which are located on each side of the uterus.
- Uterine cancer begins in the uterus, the pear-shaped organ in a woman’s pelvis where the baby grows when she is pregnant.
- Vaginal cancer begins in the vagina, which is the hollow, tube-like channel between the bottom of the uterus and the outside of the body.
- Vulvar cancer begins in the vulva, the outer part of the female genital organs.
What Are the Symptoms?
Common Symptoms of Gynecologic Cancers
- Abnormal vaginal bleeding or discharge is common on all gynecologic cancers except vulvar cancer.
- Feeling full too quickly or difficulty eating, bloating, and abdominal or back pain are common only for ovarian cancer.
- Pelvic pain or pressure is common for ovarian and uterine cancers.
- More frequent or urgent need to urinate and/or constipation are common for ovarian and vaginal cancers.
- Itching, burning, pain, or tenderness of the vulva, and changes in vulva color or skin, such as a rash, sores, or warts, are found only in vulvar cancer.
How to Reduce Gynecologic Cancer Risk?
Each type of gynecologic cancer—cervical, ovarian, uterine, vaginal, and vulvar—has its own set of risk factors. For example, cervical cancer is strongly linked to human papillomavirus (HPV) infection, while ovarian cancer risk increases with a family history of the disease. Uterine cancer is often associated with hormone imbalances and obesity. Vaginal and vulvar cancers may be linked to chronic irritation, HPV, and smoking. Regardless of the type, the risk for all gynecologic cancers generally increases with age, particularly after menopause, as hormonal changes and accumulated exposure to risk factors over time contribute to the likelihood of developing cancer.
Make An Appointment
Other type of Cancer
HPV Vaccine
Cervical, vaginal, and vulvar cancers are caused by the human papillomavirus (HPV), a very common sexually transmitted infection. The HPV vaccine protects against the types of HPV that most often cause cervical, vaginal, and vulvar cancers.
- HPV vaccination is recommended for preteens aged 11 to 12 years, but can be given starting at age 9.
- HPV vaccine also is recommended for everyone through age 26 years, if they are not vaccinated already.
- HPV vaccination is not recommended for everyone older than age 26 years. However, some adults age 27 through 45 years who are not already vaccinated may decide to get the HPV vaccine after speaking with their doctor about their risk for new HPV infections and the possible benefits of vaccination. HPV vaccination in this age range provides less benefit, as more people have already been exposed to HPV.
If vaccination is started before age 15, a two-dose schedule is recommended, with the doses given 6 to 12 months apart. For people who start the series after their 15th birthday, the vaccine is given in a series of three shots.
HPV vaccination prevents new HPV infections, but does not treat existing infections or diseases. This is why the HPV vaccine works best when given before any exposure to HPV. You should get screened for cervical cancer regularly, even if you received an HPV vaccine.
Screening Tests
Screening is when a test is used to look for a disease before there are any symptoms. Cancer screening tests are effective when they can find disease early, which can lead to more effective treatment. (Diagnostic tests are used when a person has symptoms. The purpose of diagnostic tests is to find out, or diagnose, what is causing the symptoms.)
Types of Treatment
Gynecologic cancers are treated in several ways. It depends on the kind of cancer and how far it has spread. Treatments may include surgery, chemotherapy, and radiation. Women with a gynecologic cancer often get more than one kind of treatment.
- Surgery: Doctors remove cancer tissue in an operation.
- Chemotherapy: Using special medicines to shrink or kill the cancer. The drugs can be pills you take or medicines given in your veins, or sometimes both.
- Radiation: Using high-energy rays (similar to X-rays) to kill the cancer.
